Fighting the flu
Published 12:54 pm Tuesday, October 10, 2017
With more than a dozen laboratory-confirmed cases of the flu in Clark County already, and more statewide, officials are warning the Commonwealth that flu season has arrived, and earlier than usual.
By mid-September, doctors began confirming flu cases around the state, and according to Teresa Daniels, market director of infection prevention at Clark Regional Medical Center and Bourbon Community Hospital, 13 cases have already been confirmed in Clark County between Sept. 1 and Oct. 4.
“We had three type A, 10 type B and one case of type A and B positive,” she said. “In our service area, we begin to see positive influenza screens typically in September with cases peaking in January through March.”
Anne Hatton, clinical nurse administrator at Clark County Health Department, said while flu cases can be detected year-round in the U.S., the virus is more prevalent in the fall and winter months.
“The exact timing and duration of flu seasons can vary, but influenza activity often begins to increase in October,” she said. “Most of the time, flu activity peaks between December and February, although activity can last as late as May.”
What is the flu?
The Centers for Disease Control and Prevention (CDC) has become the primary source of information about influenza, how to prevent it, how the season is affecting the U.S. and more.
According to the CDC, influenza, more commonly referred to as the flu, is a contagious respiratory illness caused by various viruses.
These viruses infect the nose, throat and lungs causing mild to severe illness. Severe cases can lead to death, especially if untreated or in certain vulnerable populations.
There are two main types of the virus: A and B. These are the strains of the flu that typically spread form person to person and are responsible for seasonal flu epidemics each year. These types can be broken down into subtypes which can also circulate and cause illness.
Hatton said the virus usually causes fever and chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches and fatigue.
“Some people may have vomiting and diarrhea, though this is more common in children than adults,” she said.
Hatton said the symptoms are similar to those of a common cold or other season illness. A test can confirm if flu is the cause for the illness, but some symptoms are cause for greater concern, she said.
“You would want to seek attention immediately for difficulty breathing, not able to drink fluids, severe or persistent vomiting, fever with rash, pain in the chest or abdomen, confusion or sudden dizziness,” she said.
Daniels’ recommendations are similar.
Emergency medical attention should be sought for children who experience, “Fast breathing or trouble breathing, Bluish skin color, Not drinking enough fluids, Not waking up or not interacting, Being so irritable that the child does not want to be held, if Flu-like symptoms improve but then return with fever and worse cough or Fever with a rash,” she said.
In adults, concerns would be difficulty breathing or shortness of breath, pain or pressure in the chest or abdomen, confusion, sudden dizziness, severe or persistent vomiting, flu-like symptoms that improve but then return with fever and worse cough, she said.
Daniels said other complications can include pneumonia, bronchitis, sinus infections, ear infections and even death.
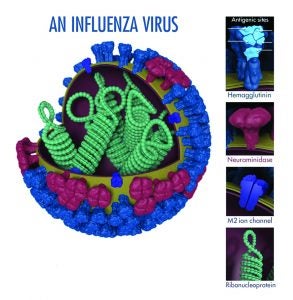
This CDC image shows the different features of an influenza virus, including the surface proteins hemagglutinin (HA) and neuraminidase (NA). Following influenza infection or receipt of the vaccine, the body’s immune system develops antibodies that recognize and bind to “antigenic sites,” which are regions found on an influenza virus’ surface proteins. By binding to these sites, antibodies neutralize flu viruses, preventing them from causing further infection.
The burden of influenza
CDC monitors circulating flu viruses and their related disease activity and provides influenza reports called FluView each week from October through May. The reports run a week behind, so the first FluView for the 2017-18 season won’t be available until next week.
The number of cases, hospitalizations and deaths caused by flu varies from year to year.
Flu seasons vary in severity depending on a number of factors including the characteristics of circulating viruses, the timing of the season, how well the vaccine is protecting against influenza infection and how many people got vaccinated.
CDC estimates influenza has resulted in between 9.2 million and 35.6 million illnesses, between 140,000 and 710,000 hospitalizations and between 12,000 and 56,000 deaths annually since 2010.
Because the impact varies, it is difficult to predict what this flu season will be like.
While flu spreads every year, the timing, severity and length of the season varies from one year to another.
Hatton shared information from Dr. Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases in the U.S.
He predicts the U.S. “will experience a similar flu season to what the Southern Hemisphere got in the season immediately preceding us. This could mean that the north will most likely experience a bad flu season.” He notes, however, that “with influenza, it is never 100 percent.”
An Associated Press article from Sept. 28 points to a similar outlook.
According to the article, “The Southern Hemisphere, especially Australia, was hit hard over the past few months with a flu strain that’s notorious for causing severe illness, especially in seniors. And in the U.S., small clusters of that so-called H3N2 flu already are popping up.”
“We don’t know what’s going to happen but there’s a chance we could have a season similar to Australia,” Dr. Daniel Jernigan, influenza chief at the U.S. Centers for Disease Control and Prevention, told The Associated Press.
The virus got an early start in Kentucky with two cases confirmed in Jefferson County as early as Sept. 15.
Spreading the virus
With an early start and potentially bad outlook, health officials at the state and local level are advising people about how the virus spreads and how to prevent spreading it to others.
Most experts think influenza spreads primarily through small droplets containing the virus, which are expelled into the air or onto surfaces when people with the virus sneeze, cough or even talk.
These droplets can land in the mouths or nose of others or be picked up through contact with infected surfaces and transferred from person to person.
Once these droplets containing the virus are transferred, a complicated process takes place which allows the virus to infect the cells, marking the beginning of the infection
The virus is generally transmitted from person to person, but in some cases, the virus can be spread from animals to people. Influenza A viruses are found in many different animals, including ducks, chickens, pigs, whales, horses and seals. This includes the strains referred to as swine flu transmitted by pigs and avian flu transmitted from birds.
Certain populations, including pregnant women, people 65 or older, children 5 or younger, long-term care residents and American Indians and people of Alaskan Native decent are more susceptible to the virus, Daniels said.
According to the CDC, people with asthma, lung disease, sickle cell disease, diabetes, cancer, HIV, and kidney and liver disorders are at high risk for developing complications.
Protecting against the flu
Getting an annual flu vaccine is the first and best way to protect against the influenza virus.
“Getting the flu can be debilitating and sometimes life-threatening,” said Dr. Hiram C. Polk, Jr., Kentucky’s public health commissioner. “Vaccination is the best tool we have to prevent the flu.”
Traditionally the flu vaccine is available as an injection or a nasal spray. However, this year, the CDC recommends only the injectable vaccine.
The flu virus is constantly evolving, requiring that the composition of U.S. flu vaccines be reviewed annually and updated as needed to match circulating flu viruses.
The CDC recommends that everyone six months of age or older receive the flu vaccination.
“Optimally, vaccination should occur before the onset of influenza activity in the community, ideally before the end of October,” Hatton said.
Flu vaccines protect against the three or four viruses (depending on vaccine) that research suggests will be most common. For 2017-2018, the vaccines are recommended to protect against two subtypes of type A and two subtypes of type B influenza.
If you contract a strain not included in the vaccine, some protection is still provided.
“A less than optimal match may result in reduced vaccine effectiveness against the virus that is different from what is in the vaccine, but it can still provide some protection against influenza illness,” Elizabeth Lovell, director of pharmacy at CRMC, said. “Flu vaccines cause antibodies to develop in the body about two weeks after vaccination. These antibodies provide protection against infection with the viruses that are in the vaccine.”
For the 2017-2018 season, manufacturers projected they would provide between 151 million and 166 million doses of injectable vaccine for the U.S. market, according to the CDC.
Flu vaccines are already available, and are offered by many doctor’s offices, clinics, health departments, pharmacies and college health centers, as well as by many employers, and even by some schools.
The body’s immunity to the virus provided by the vaccine declines over time, so it is important that people get the vaccine every year for optimal protection.
In Clark County, Clark Regional Medical Center and the Clark County Health Department are among the various agencies offering the vaccine this year.
Side effects including soreness, redness, swelling at the injection site, a low-grade fever and some aches are toe be expected, Lovell said, but are usually mild and short-lasting.
“The biggest misconception is that the flu vaccine will cause the flu,” Lovell said. “It is not possible for people to ‘catch the flu’ from the flu vaccine.”
Other preventative measures
In addition to getting a seasonal flu vaccine, people can take other steps on a day-to-day basis to prevent the spread of the illness.
“Cover your cough. Cough into your arm instead of your hand. Perform hand hygiene with soap and water 15 to 20 second lathering or use hand sanitizer. Get your flu vaccine. Stay home if you are ill,” Daniel said. “Your eyes, nose and mouth ( also known as your T-zone) is the point of entry for virus. Because of this, you want to protect your T-zone from contamination from your hands, or other peoples’ coughs and sneezes.”
If someone suspects they have the flu, Daniels recommends seeing a doctor to get an antiviral medication called Tamiflu to treat the illness.
“Tamiflu is an antiviral medication that can be used to help lessen the symptoms if someone has a confirmed case of the flu,” Lovell explained. “If you have the flu the best thing to do is stay home, rest and stay hydrated.”
Practices to prevent spreading the flu
— Avoid close contact with sick people. When you are sick, keep your distance from others.
— Stay home when you are sick to prevent spreading the virus.
— Cover your mouth and nose with a tissue or your elbow when you cough or sneeze.
— Wash hands with soap and hot water for about 30 seconds and dry thoroughly. Wash your hands frequently and use hand sanitizer between washes.
— Avoid touching your eyes, nose or mouth, as germs are often spread by touching contaminated objects and then rubbing these parts of your body.
— Clean and disinfect your home, office and school often, especially when someone has been sick.
For detailed information about the 2017-18 flu season, visit https://www.cdc.gov/flu/about/season/flu-season-2017-2018.htm.